In the Flow (by Dr. Hari Bhajan
Singh Khalsa---Dr. Mha Atma's chiropractor)
Imagine a river flowing powerfully through
the land. Your mind is like that river-carrying your thoughts, memories,
ideas and self-awareness through the landscape of your Being. You can
harness the power of your mind, in order to nurture your body, mind and
spirit just as water nourishes the plants. Your mind acts as a powerful
ally to help you achieve your goals and dreams. Unchecked, it can reap
destruction, much like a flood.
Meditation is a time-tested technique for
controlling the flow of the mind. Over the ages, yogis and sages have
developed ways to channel the mind's power for healing and inner peace.
Today, you can spend time and money on self-help courses, therapy and
doctors, but meditation can also be a daily practice to bring to bear
all the gifts that the mind has to offer. You can grow your perceptions,
feelings and visions in a way that will shower you with calmness,
clarity and purpose. So pull up your meditation mat, engage your mind
and flow gently down the stream.
---------------------------------------
A Fitter You = A Better Fighter Against COVID-19
Complications
While vaccine seems destined
to remain the buzzword when it comes to COVID, let's not
forget about natural options that, while they may not
prevent COVID-19 infection, appear to reduce the chances
you'll suffer serious consequences if you do end up
contracting the virus.
Case in point: a
new study that suggests adults who score high
on an exercise stress test are less likely to be
hospitalized due to COVID-19 compared to patients who score
lower. Patients who completed the test between Jan. 1, 2016
and Feb. 29, 2020, received a test for SARS-CoV-2 between
Feb. 29, 2020 and May 30, 2020. Among patients who tested
positive, peak metabolic equivalents of task (METs), a
measure of maximal exercise capacity, were significantly
higher in patients not hospitalized compared to patients who
were hospitalized.
The researchers' conclusion,
published along with their findings in Mayo Clinic
Proceedings, makes the value of these study results clear:
"Maximal exercise capacity is independently and inversely
associated with the likelihood of hospitalization due to
COVID-19. These data further support the important
relationship between cardiorespiratory fitness and health
outcomes."
--------------------------------------
Are Personal-Care Products Messing
With Your Hormones?
The trend away from makeup,
particularly during the coronavirus pandemic when working from home
has become the norm and nights "out on the town" have been rare, may
have a big bonus when it comes to women's health. According to new
research, teenage girls who take even a short break from cosmetics
experience a "significant drop in hormone-disrupting chemicals."
Incredibly, it took only three days for significant improvements to
be noticed.
And don't think makeup is the only
culprit to consider; according to the study, published in Environmental
Health Perspectives, avoiding personal care products including
soap, sunscreen, shampoo, conditioner and other hair products
containing chemicals such as phthalates, parabens, tricolsan and
oxybenzone appeared to be just as effective.
Specifically, the three-day switch to
lower-chemical products revealed a significant drop in chemicals in
the body, measured via urine samples. Methyl and propyl parabens
(common use: cosmetics preservatives) declined by 44 percent and 45
percent, respectively; metabolites of diethyl phthalate (common use:
perfumes) declined by 27 percent; and triclosan and benzophenone-3
both declined by 36 percent.
What's the lesson? It's just as true
about personal care products as it is about health care in general:
think natural! Always consider what you're putting into or on your
body, whether a food, medication, cosmetic or anything else.
--------------------------------------
Does Your Dental Health Impact
Whole-Body Health?
Who knew your teeth could have such a
profound influence on your overall health. New research suggests
people with poor dental hygiene leading to periodontal / gum disease
are more likely to have increased insulin resistance and other
indicators of metabolic syndrome – a constellation of risk factors
that can lead to type 2 diabetes and other health issues.
In the study, researchers correlated
infection with Porphyyromonas gingivalis, a periodontal
bacterium, with the development of metabolic syndrome / metabolic
dysfunction in skeletal muscle (which have a high metabolic capacity
that aids in glucose metabolism). They then determined that
infection may compromise the gastrointestinal microbiome, leading to
metabolic syndrome. Study findings appear in The FASEB Journal.
Metabolic syndrome is characterized by
a group of concurrent conditions that elevate the risk of not only
type 2 diabetes, but also heart disease and stroke. High blood
pressure, high blood sugar, excess abdominal body fat, and high
cholesterol / triglyceride levels are the primary conditions that
lead to a metabolic syndrome diagnosis. If you suffer from any of
the above conditions and you're not practicing good dental hygiene,
you're on the fast road for major health issues that are easily
avoided with a few simple lifestyle changes. Your doctor can tell
you more about how to avoid metabolic syndrome and enjoy lasting
whole-body health.
--------------------------------------
A Drug-Free Way to Treat Headaches:
Chiropractic Care
By Perry Nickelston, DC, FMS, SFMA
More Americans complain about
headaches than any other health condition, including back pain; in
fact, approximately 45 million Americans say they suffer headaches
each year.
That's one in every six people or more
than 16 percent of the population. More than 8 million Americans
visit their doctor seeking relief for symptoms of headaches each
year. Unfortunately, the most popular treatment is over-the-counter
pain relievers or prescription medication.
There is some good news when it comes
to headaches. There are safe and effective natural solutions
available to help reduce or eliminate the symptoms of various
headache types. For example, chiropractic treatment is a highly
sought-after alternative treatment for the debilitating effects
associated with headaches. Let's learn about that headache you may
be suffering from and how chiropractic can help you get rid of it.
Headaches 101
Tension headaches: The most
common type of headache is the tension headache. It is estimated
that 80-90 percent of the U.S. population suffers from tension
headaches at some point in their lives. There are two primary types
of tension headaches:
-
Episodic :
Headaches appear occasionally, usually less than 15 times per month.
-
Chronic :
Headaches occur more than 15 times per month or on a consistent
basis.
Tension headaches are intimately
connected to abnormal posture, muscular tightness, joint stiffness,
and restricted range of motion in the body. To obtain optimum health
and function, it is important to remember that everything is
connected and everything matters. Dysfunctional patterns of movement
and posture affect how much tension and stress your body holds. The
body must compensate for these dysfunctional patterns by any means
necessary, and it accomplishes this by altering tension points.
Muscles attach to anchor points on
bone and act as primary movers and stabilizers for your body. Mover
muscles are used get you from point A to point B, such as a getting
up out of a chair. Stabilizer muscles control that movement so you
don't fall down while standing up. Abnormal posture and altered
tension points on bone anchors puts too much wear and tear on
muscles and joints. Your brain and nervous system must compensate
for this dysfunction by altering blood flow, muscle movement
patterns and breathing. These alterations often lead to tension
headaches.
Migraines: The second most
common type of headache is the migraine headache. Approximately
16-17 percent of the population complains of migraines. These
headaches are far more debilitating than the tension-type headaches.
More women than men suffer from migraine headaches, leading
researchers to believe there may be a hormonal component to
migraines. The majority of migraine sufferers report some sort of
trigger that kicks of their headaches (food, drink, smell, etc).
How Chiropractic Can Help
Chiropractic care can help alleviate the symptoms of tension and
migraine headaches by improving and restoring normal postural
patterns. Chiropractic treatment is aimed at normalizing muscle
tension, restoring joint range of motion, and stabilizing the body
to reduce abnormal stressors. Optimizing postural control of the
head and neck reduces the workload your muscles must apply just to
keep your head up during the day. Proper spinal alignment and muscle
control helps give the body a fighting chance of avoiding a tension
headache.
Proper breathing is essential to
relaxation, blood flow, and oxygen supply to the brain and body.
Abnormal posture, which can include such dysfunctions as rounded
shoulders, neck forward over the shoulders, slouched positions and
tightness in the hips from sitting all day, decrease lung capacity.
This decreased capacity alters how much you breathe, how often, and
from where.
Headache sufferers tend to breathe
more from their chest and shoulders as opposed to their diaphragm.
This leads to repeated elevation of the shoulders and upper back
muscles hundreds of times a day, leading to increased tension in the
head and neck. Chiropractic restores function to the spine, ribs,
and hips to maximize breathing and good postural control. Better
breathing equals better health.
If you're suffering from headaches and
are tired of taking pain-relieving medication day after day, your
doctor of chiropractic will work closely with you to determine
likely triggers for your headaches and make subtle changes in your
activities of daily living to empower you to take back control of
your life.
--------------------------------------
Surgery: The Ultimate Placebo
By Ronald Feise, DC
(Note from Dr. Mha Atma: This
article was written for chiropractors but I wanted to share it with
you--quite understandable.)
A patient tells you his father has had
low back pain for several years and has tried many treatments, but
nothing has helped. Spinal fusion has been recommended. Complicating
matters, his father lives on the other side of the country. How do
you respond? What does the current research demonstrate?
Obviously, you want to get his father
into the hands of a competent chiropractor who can do a
comprehensive case history and examination, and determine whether he
can be helped with chiropractic treatment. To facilitate this
process, you want to provide your patient with some relevant
research. Fortunately, a recently published resource addresses this
type of surgery, among others.
What an Orthopedic Surgeon Says
About Spinal Surgery
The book is "Surgery, The Ultimate Placebo" by Dr. Ian Harris (1) –
not only a practicing orthopedic surgeon, but also a professor of
orthopedic surgery. He is a widely published research scientist and
expert on spinal fusion. The book is well-researched and written in
a very approachable manner. Here's what Dr. Harris says about spinal
surgery:
"[T]here is very little evidence that
spine fusion surgery for back pain is effective. It is very
expensive, often leads to complications, often requires further
surgery, is associated with increased mortality, and often does not
even result in the spine being fused."
"Millions of people have had spine
fusions for back pain, and I am not at all convinced that the
benefits of this surgery outweigh the considerable harms."
"Somebody is winning here, and it
isn't the patients."
This information is important not only
for this patient's father, but also your entire practice. (You might
consider having a copy of the book in your reception room, with
pertinent pages marked for easy reference.)
Spine Surgery: Important Facts to
Understand and Share With Patients
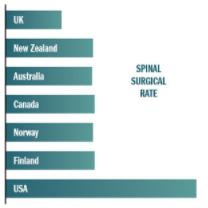
In addition to Dr. Harris's book, you
can also provide some additional facts about spinal surgery. (See
the "Spinal Surgical Rate" chart.) The U.S. has the highest rate of
cervical and lumbar spine surgery in the world – roughly 200 percent
that of New Zealand, Australia, Canada, Norway and Finland, and 340
percent of that of the U.K.
You might assume that Americans must
have higher rates of spinal pain or more severe conditions, but you
would be wrong. There are no biological differences from country to
country, and epidemiological studies demonstrate that rates of neck
and back pain are similar among geographic areas. Could surgeon
profits be the underlying cause of excessive surgeries?
Serious adverse events caused by
spinal surgery are remarkably common. Several published studies
conducted by independent medical research teams found that the
reoperation rate (failure rate) for spinal surgery is greater than
22 percent (2) Serious postoperative pain and disability can be
experienced by more than 29 percent of patients.(3-4) Death rates
following spinal surgery are about 1 per 1,000 operations, and
blindness following spinal surgery is estimated at more than 1 per
1,000 operations.(5-7)
Can you imagine if chiropractors had
death rates at 1 per 1,000 patients? Keep in mind, both professions
do not treat dissimilar patient populations.
Spinal surgeons have failed to
demonstrate benefit for spinal surgery related to disc degeneration,
disc herniation, or neck or back pain. To date, spinal surgeons have
failed to provide scientific evidence of surgical effectiveness
sufficiently large to meet the FDA threshold for clinically
meaningful benefit.
References
-
Harris I. Surgery, The Ultimate Placebo: A Surgeon Cuts Through the
Evidence. University of New South Wales Press, 2016.
-
Kim CH, et al. The long-term reoperation rate following surgery for
lumbar herniated intervertebral disc disease: a nationwide sample
cohort study with a 10-year follow-up. Spine, 2019;44:1382-1389.
-
Ohnmeiss DD, et al. Effect of adverse events on low back surgery
outcome: twenty-four-month follow-up results from a Food And Drug
Administration investigational device exemption trial. Spine,
2010;35:835-8.
-
Pieber K, et al. Predictors of an unfavorable outcome 1.5 and 12
years after a first, uncomplicated lumbar disc surgery. Eur Spine J,
2016;25:3520-3527.
-
Myers MA, et al. Visual loss as a complication of spine surgery. A
review of 37 cases. Spine, 1997;22:1312-1319.
-
Roth S, Barach P. Postoperative visual loss. Still no answers - yet.
Editorial views. Anesthesiology, 2001;95:575-577.
-
Wang MC, et al. Complications and mortality associated with cervical
spine surgery for degenerative disease in the United States. Spine,
2007;32:342-7.